|
Percent change (and 95% confidence interval) in incidence of laboratory-confirmed bacterial and parasitic infections in 2011* compared with average annual incidence for 1996–1998 and for 2006–2008, by pathogen, Foodborne Diseases Active Surveillance Network (FoodNet), United States |
|||||
|
|
1996–1998 comparison period |
2006–2008 comparison period |
|||
|
Pathogen/Syndrome |
% change† |
(95% CI) |
% change† |
(95% CI) |
|
|
Campylobacter |
22%↓ |
(15%↓ – 28%↓) |
14%↑ |
(7%↑ – 21%↑) |
|
|
Listeria§§ |
35%↓ |
(15%↓ – 50%↓) |
8%↑ |
(14%↓ – 35%↑) |
|
|
Salmonella |
1%↓ |
(8%↓ – 7%↑) |
6%↑ |
(0.5%↓ – 12%↑) |
|
|
Shigella |
65%↓ |
(51%↓ – 75%↓) |
43%↓ |
(25%↓ – 56%↓) |
|
|
STEC¶ O157 |
42%↓ |
(28%↓ – 53%↓) |
25%↓ |
(11%↓ – 37%↓) |
|
|
STEC non-O157 |
NA** |
|
NA |
||
|
Vibrio |
76%↑ |
(30%↑ – 137%↑) |
15%↑ |
(8%↓ – 44%↑) |
|
|
Yersinia |
52%↓ |
(38%↓ – 62%↓) |
5%↓ |
(24%↓ – 18%↑) |
|
|
Cryptosporidium |
24%↑ |
(17%↓ – 88%↑) |
27%↑ |
(4%↓ – 68%↑) |
|
|
Cyclospora |
NA |
NA |
|||
|
HUS†† |
NA |
7%↓ |
(33%↓ – 28%↑ ) |
||
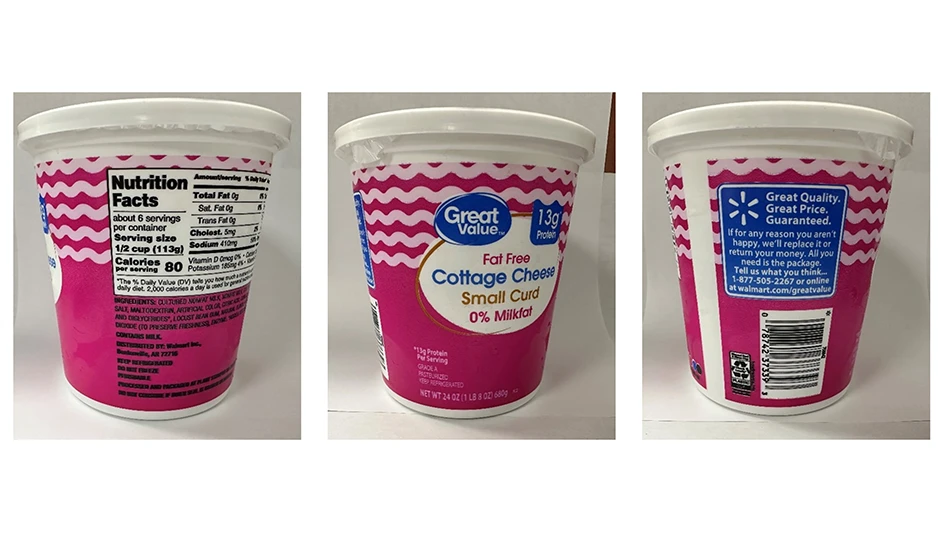
- The overall frequency of illnesses caused by the six most common foodborne diseases (Campylobacter, Listeria, Salmonella, Shiga toxin-producing E. coli (STEC) O157, Yersinia and Vibrio) was 23% lower in 2010 than in 1996-1998. However, a comparison of 2006-2008 to 2010 indicates that progress has slowed recently. (See table)
- Salmonella Enteritidis infections are a growing problem in the United States; chicken and eggs are likely major sources.
- Fourteen percent of the illnesses caused by the seven most common foodborne diseases are attributable to contact with animals.
- The overall frequency of illnesses caused by Campylobacter, Listeria, Salmonella, Shiga toxin-producing E. coli (STEC) O157, Yersinia and Vibrio was 23% lower in 2010 than in 1996-1998. However, a decrease in incidence between 2006-2008 and 2010 of 3% indicates that progress has slowed recently.
- In 32 % of foodborne disease outbreak investigations conducted by FoodNet sites, 2003–2008, the food vehicle was determined, although the etiology (bacteria or virus responsible for the outbreak) was found in 60% of outbreak investigations. Investigations that were not successful in determining the food or cause of the outbreak had too few patients ill, too few stool specimens to test or too few control subjects.
- Campylobacter is the most common cause of foodborne illness in travelers returning to the United States from overseas. Over half of all travel associated infections reported were in travelers to Latin America and the Caribbean. However, travel to Africa carried the greatest risk of travel associated infection (75.9 cases per 100,000 travelers).
- Fourteen percent of all illnesses (445,213 annually) caused by the seven most common foodborne diseases are attributable to contact with animals: direct contact with wild animals, pets, and other animals, as well as indirect contact with the animal’s feces, bodily fluids or its environment. Campylobacter, Salmonella, and Cryptosporidium caused the majority of illnesses, hospitalizations and deaths attributed to contact with animals and their environments.
- There was no significant change in the incidence of listeriosis from 2004 to 2009. Increasing prevention efforts such as food safety education among pregnant women, especially those who are Hispanic, and older adults are recommended to substantially decrease overall rates of listeriosis.
- Older adults and pregnant women, especially Hispanics, have a higher risk of invasive diseases caused by Listeria infections, including bloodstream infection, meningitis, and miscarriage and stillbirth. Among older adults, the risk of invasive listeriosis increases as people get older.
- The frequency of Vibriosis illness increased from 1996 to 2010, according to data from both Vibrio and FoodNet surveillance systems. More effective prevention efforts such as measures to inform the public about the hazards of raw shellfish consumption and measures to decrease contamination of oysters are recommended to decrease rates of vibriosis.
- Resistance to commonly used antibiotics is high. Although most cases of shigellosis can be managed without antibiotics, it may be more difficult to treat severe infections if Shigella isolates are becoming resistant to commonly used antibiotics.
- Infections from Salmonella serotype Enteritidis are a growing problem in the United States. Chicken and eggs are likely major sources.
- Culture-independent testing is becoming a more common way to diagnose foodborne diseases, and with it comes challenges and opportunities for public health agencies, clinical laboratories and industry. This report summarizes these challenges and opportunities, and suggests strategies that can be adopted to ensure that surveillance data continues to be accurate. Some of the strategies suggested for public health agencies include collecting information on testing methods used, regularly surveying clinical laboratories regarding testing practices, and conducting validation studies.
- There is a need to develop recommendations for best practices for Campylobacter diagnostic testing. Although most laboratories are using culture-based methods to identify Campylobacter infections, procedures differ widely and most labs do not adhere to existing guidelines, likely resulting in under-diagnosis.
Latest from Quality Assurance & Food Safety
- Director General of IICA and Senior USDA Officials Meet to Advance Shared Agenda
- EFSA and FAO Sign Memorandum of Understanding
- Ben Miller Breaks Down Federal Cuts, State Bans and Traceability Delays
- Michigan Officials Warn Recalled ByHeart Infant Formula Remains on Store Shelves
- Puratos USA to Launch First Professional Chocolate Product with Cultured Cocoa
- National Restaurant Association Announces Federal Policy Priorities
- USDA Offloads Washington Buildings in Reorganization Effort
- IDFA Promotes Andrew Jerome to VP of Strategic Communications and Executive Director of Foundation