When I say that I am trained as a food microbiologist, what I really mean is that I’m trained in bacteriology. Pathogens like Salmonella, E. coli, Listeria and the like continue to cause major challenges for fresh produce, but I am confident that with increased education, training, implementation of strong programs, and financial resources to support these improvements, we can address these issues. I am less confident when it comes to our ability to control Cyclospora cayetanensis.
Cyclospora is a parasite. Each spring, on a very predictable basis, more than 1,000 Americans are diagnosed with cyclosporiasis. While the illness is not known to be deadly, it’s still quite unpleasant, and something we need to address. And “we” is the collective we, not just the produce industry. Cyclospora is a public health issue, not a produce issue, and not even a food issue. Humans are the only known host for the organism, and the parasite seems to be endemic to some populations. Until this is addressed as a public health issue, Cyclospora will continue to use produce, and likely other food and non-food vehicles, to continue causing illness.
A collaborative approach to addressing the problems outlined here will come only if we dispel the myth that Cyclospora presence is indicative of poor human hygiene. The complexity of the outbreaks over the past several years, the findings of Cyclospora on produce grown in the U.S. and in U.S. waterways, and the major blind spots that exist when it comes to the ecology of this microorganism, suggest that this is not your “typical” fecal-oral associated pathogen.
Perhaps the biggest impediment to better understanding this elusive parasite is that ironically, despite the high burden of illness, we don’t have enough Cyclospora material to study. Supply is quite limited. Unlike bacteria, Cyclospora does not grow outside a human host. You cannot stick a little in a test tube and have abundant Cyclospora the next morning. The only Cyclospora we have are the ones harvested from stool samples of ill individuals.
Another major challenge when assessing the risk of Cyclospora is that we currently lack the means to correlate detection with risk. The organism has a complex life cycle and is presumed to require a week or two outside the human host before it morphs into its infectious form. However, the “gold standard” detection method is based on PCR, which detects DNA. Many microbial methods employ the same basic principles but are preceded by an enrichment step to get sufficient numbers of organisms, from which one can infer that the organism had to be alive in order for it to replicate. Not Cyclospora. There is no replication, so we’re left to wonder if the detected DNA is from Cyclospora that is alive or not.
From the standpoint of public health, it’s prudent to assume that the detection of DNA could signal the presence of the live pathogen. Still, with so little material to work with, genetic typing generally cannot be done on food or water samples. This means we cannot link environmental or product findings to cases of illness. (Cases can be linked to each other, although not yet in real time, because unlike product and water samples there is sufficient Cyclospora in stool samples.)
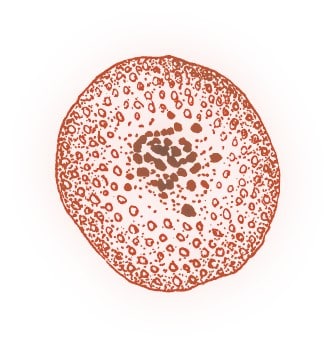
Discerning infectivity and the public health risk are greater challenges. Currently, microbiological analysis is the only way to determine the physiological state of the parasite. It takes a well-trained eye, since other parasites may look similar under the microscope, and since there are species of Cyclospora other than cayetanensis (which is the one of human concern).
Even if infective Cyclospora is found, we don’t know exactly how to kill it. You can’t thermally process produce and still eat it raw. Parasites are larger than bacteria and should be able to be removed more easily via filtration, however that isn’t practical in every circumstance. Beyond that, the limited supply of oocysts for research, limited number of researchers, and difficulties in interpreting methods means that we are in our infancy when it comes to understanding the vulnerabilities of this organism.
If we work together in a deliberate, systematic manner we can make progress. We have to; we have no choice. Because outbreaks have historically been linked with fresh produce, the industry has taken the lead in coordinating a multi-institutional, public-private collaboration to prioritize research needs over the next several years.
Jennifer McEntire, Sr. Vice President Food Safety & Technology, United Fresh
Explore the November December 2020 Issue
Check out more from this issue and find you next story to read.
Latest from Quality Assurance & Food Safety
- FDA Publishes Landmark Final Rule to Enhance the Safety of Agricultural Water
- The Wendy's Company Reports 2023 Corporate Responsibility Progress
- Local Bounti Opens New Controlled Environment Agriculture Facility
- Tröegs Partners with Patagonia Provisions to Introduce Kernza Lager
- Neogen Launches New Molecular Method for Detection of Two Salmonella Serotypes
- Standard Meat Company Appoints Keith Blanks as Chief Commercial Officer
- USDA Finalizes Policy to Protect Consumers from Salmonella in Raw Breaded Stuffed Chicken Products
- Comedian Vanessa Bayer Explores the World of Dairy Farming in ‘Dairy Diaries’




